A large number of people fall on the lower back, and when the load is lifted, twisted, from a long static position, additional pressure will be created in it. Excessive load, a constantly wrong lifestyle leads to a decrease in the musculoskeletal system: the vertebrae and discs between them, which serve as shock absorbers. From now on, it is necessary to find information about lumbar spine osteochondrosis: symptoms and treatment. Why is there a deterioration of the spinal joints?

Deterioration of the musculoskeletal system occurs as follows: natural shock absorber in the spinal space loses its elasticity, shrinks, spreads beyond its natural limits, pressure from the spine, organs, other ligaments also increases. Let us explain those who tend to acquire such pathologies. Osteochondrosis of the lumbar spine can be observed in people:
- Which of the early generations suffered similar suffering;
- Having hormonal disorders;
- Individual tendency to develop such diseases (e. g. , congenital structure of the spine);
- Those who neglect proper nutrition. On the table, every day one should get a balanced diet with fats, vitamins, healthy protein;
- Those who have inactive jobs: sitting long or standing long in one place;
- Experiencing sharp and heavy loads on the spine, for example: weightlifting, loaders, people during gardening;
- Suffering from digestive, metabolic, pelvic organs;
- Trauma (pulled too hard in the back, hit to the side, fell, bent);
- Has reached the age of 30;
- Diabetes.
If there are signs of lumbar osteochondrosis, described in the section below, then some habits should be avoided:
- slouch;
- asap;
- take a bent pose for a long time;
- moves slightly;
- drinking alcohol;
- sitting without a break at work;
- dress not for the weather, let the body cool.
Important. Any disruption to the ligaments is exacerbated by the presence of excess weight. With excess weight, the load on the lower body increases, and the lumbar region, which is overgrown with fat, is massaged massively.
The stage of the disease, its symptoms
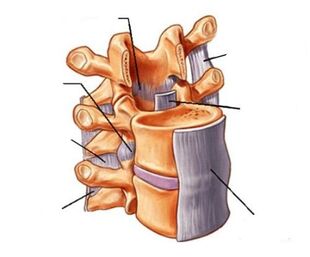
Initially, there is periodic mild pain that increases with physical exercise. This discomfort indicates that it is time to observe lumbar spine osteochondrosis. Nowadays, the intervertebral disc (the spinal disc is the channel through which the spinal cord and the fibrous ring around it) degenerates. Further, the distance between the vertebrae is reduced, the nerves are pinched. The pain becomes severe, grabbing not only the back, but also the hip, gluteal muscles. In the third stage, the fibrous ring is shattered, leading to the formation of a spinal hernia, irreversible cavities, and constant pain. The fourth stage leads to disability. Special classifications of lumbar spine osteochondrosis include:
- sick;
- ischemic syndrome;
- radicular syndrome;
- vertebral syndrome;
- too many tissue confirmations.
Pain sensations have different levels and properties of severity: lumbago, for example, is called lumbago; persistent, exacerbated by stress, lumbodynia; spread in the lower part of the body is called lumboischialgia. If back pain is not addressed, the vertebrae acquire free movement in the spinal space. There is compression of the nerve root when lifting the load and acting abruptly, then the pain from the lower back disappears, but moves to another part of the body, to which the nerves are responsible. Unconsciously, we change position, adjusting so that there is a little pain in the back, but this definitely changes the walking style and bends of the spine. All of this refers to radicular syndrome, which begins as irritation, and then becomes inflamed. Signs of lumbar spine osteochondrosis with radicular syndrome:
- Excessive fatigue in the back muscles;
- back bend changes;
- walking style changes;
- swelling of the lower extremities;
- pain in one or both legs;
- severe pain;
- temporary loss of leg sensitivity;
- chronic constipation periodically;
- men have problems with happiness;
- menstrual irregularities in women;
- body intoxication;
- blood stagnation.
You can see that during rest, painful sensations arise, and when doing exercises on the back, they subside. Already at this stage, it is necessary to find a doctor: chiropractor, surgeon, neurologist, traumatologist (because the causes of lumbar spine osteochondrosis include trauma). If you let the disease continue, the problem will increase, plus different friends:
- hot;
- numb;
- sweating;
- tingling;
- shivering;
- goosebumps;
- impotence;
- intestinal colic.
The back muscles lose tone, and this causes loss of human motor function in general. With very dangerous radicular syndrome, paralysis will occur. Ischemic syndrome is associated with radicular. At first, squeezing the bloodstream is periodic, but then squeezing it causes cramps. You can see it while walking normally - you walk in pain, if you stop, it does not hurt. The main deterioration occurs inside and is invisible to the naked eye - blood flow does not provide the necessary supply to all pelvic organs. Painful sensation in the back, thighs may occur, then gluteal muscle paralysis may occur. Vertebral syndrome already involves changes in the skeleton, the blood vessels themselves.
Important. Symptoms of lumbar osteochondrosis in women are associated with a hormonal background, physiological characteristics of the body. The occurrence of pain, incorrect posture is influenced by wearing inappropriate shoes: on the soles of the feet that are too hard or too soft; the heel is too high or the heel is too low.
Diagnostic stage of the disease

It is very difficult for a doctor to classify and name the stage of the disease during an external examination. Initially, the neurologist can diagnose:
- constant curvature of the spine;
- pain when touching;
- decrease in walking distance;
- gluteal asymmetry;
- Michaelis diamond change.
But the most accurate diagnosis can only be made with the result:
- computed tomography (CT). The most optimal option for determining the stage of development of the disease, it is possible to assess the degree of decline of the spinal column.
- X-ray imaging. According to them, it is possible to determine the presence of disease, but it is not always possible to determine the degree of development of damage to nerve fibers and blood vessels.
- magnetic resonance imaging. Quite a long time (from half an hour to an hour), an expensive procedure, which also provides the most complete details of what happens to the nerve roots and blood vessels.
Thus, doctors can finally assess the lumbar spine osteochondrosis: symptoms and treatment only with the results of apparatus studies. Low back pain, unrelated to intervertebral disc violations, caused by the flu, kidney, menstrual cycle, or back muscle pain.
Important. CT, X-ray examination is not acceptable for pregnant women. CT is not safe for: 1) children under 14; 2) people with iodine allergies.
Medical treatment
The causes of the onset of the disease, its characteristics have been considered above, now let us move on to the second point of lumbar spine osteochondrosis: symptoms and treatment. The longer you ignore the body signals, the sooner the disease will go away. The farther from the beginning, the more medications and procedures to be used. Treatment objective:
- identify, eliminate the causes of pinching the roots, spinal blood vessels;
- restores skin sensitivity;
- to prevent the development of pathology;
- start body processes for self-healing;
- strengthens one's muscle tone;
- restores the function of the internal organs of the small pelvis;
- restores the normal flow of the lumbar vertebra.
If you experience any discomfort, see your doctor. The first thing to do at the first symptom is to pay attention to: the bed (a variety of orthopedic mattress options that must be chosen individually), pillows (may not suit your size or softness), position during sleep, motor activity. At home, without being examined by a doctor, osteochondrosis of the lumbar spine is only treated with bed rest. Therefore, a visit to the doctor is mandatory. At the stage of remission and the acute phase of the disease, different medications are taken. In the final phase, the drug is used to relieve pain, release nerves from the vertebral mites, and eliminate inflammation. Determine: - restrictions; - glucocorticoids; - chondroprotectors; - myo-julap; - Nonsteroidal anti-inflammatory drugs (NSAIDs).

The last group of drugs, in addition to relieving pain, fights against excessive body temperature, edema, inflammation. Such funds can be: rectal, for internal use, injection, external. Treatment of lumbar spine osteochondrosis most often begins with NSAIDs:
- Diklofenak;
- Piroksikam;
- Ibuppofen;
- Himeculide;
- Hapoksi;
- Decketoprofen;
- Meloksikam;
- Aceclofenac.
The anti-inflammatory drugs on this list are various ointments, tablets, gels. Some NSAID tablets have contraindications for those with ulcers or gastritis. Muscle relaxation relaxes joint spasms and accidental contraction of the back muscles by temporarily reducing muscle tone. This group of drugs includes tizanidine, tolperisone hydrochloride. When there is an opportunity to save the intervertebral disc, chondroprotectors are prescribed, which serve to restore the annulus fibrosus. How to take such a group of drugs is very long - at least 1. 5 months, and the results can be seen only after one year. They try to avoid glucocorticoid intake, as they have side effects when taking it, as this group of drugs belongs to the steroid hormone. They must be taken under the supervision of the attending physician in compliance with all prescriptions, as only a specialist knows how to cure lumbar osteochondrosis. An example of such a drug is hydrocortisone. Blockage is not a cure in itself, but it is a powerful local pain reliever. The technique is as follows: the introduction of injectable painkillers (IO) or the combination of IO with drugs from the glucocorticoid group in the pain area. The blockage has no medicinal properties, but can be addictive, which will lead to loss of sensitivity to these drugs. If injected frequently, the muscles around the injection may develop atrophy. Therefore, when acute pain is reduced with this method of treatment, patients are given medications designed to restore damaged tissue, blood flow, and help improve muscle and nerve fiber tone. This:
- Chondroprotectors, which have a general strengthening effect on bone tissue, normalize cartilage tissue metabolism.
- Vitamins that help restore nerve patency.
- Biogenic preparations that encourage the body to heal on its own;
- Varicose veins that thin the blood to improve the nutrition of internal organs.
During treatment, along with the main medication, antidepressant medications are prescribed. Here is how to treat lower back pain while relieving acute pain:
- use external heating, analgesic, anti-inflammatory agents;
- do special exercises for the back;
- go massage;
- lead a gentle lifestyle for the back;
- wear a belt corset while exercising.
Massage, exercise therapy, physiotherapy and alternative treatments.

An inexpensive effective method for combating shock absorption reduction is physiotherapy, massage, physiotherapy training. The actual massage can only be done by a professional with a medical education, so a simple visit to a beauty salon is not suitable for patients. Each stage of the disease requires different stresses and techniques. With proper therapy, muscle spasms disappear, the back muscle skeleton is strengthened, and pain gradually disappears. Physiotherapy only occurs in the process of reducing painful processes or when they are absent (to maintain spinal movement). Gymnastics is selected individually, based on the age, condition of the person, the stage of disease development. The productivity of therapeutic training directly depends on the quality of performance and frequency: training must be done systematically. It is recommended to relax at home, lying on your back, bending your legs, placing a small roller under your lower back. The healing process is monitored with the help of X-rays, tomographic surveys. Physiotherapy treatment is prescribed during remission and exacerbation. Methods such as:
- acupuncture. Ancient method of treating pain, based on the stimulation of acupuncture points with fine needles. The procedure relieves cramps, reduces pain, eliminates them completely, reduces tissue edema;
- Ultraviolet radiation, which stimulates the body to absorb calcium;
- ampilpus, named from the appropriate device. The treatment procedure is as follows: the equipment plate is mounted on the back, and the therapeutic current corresponding to the different parameters flows through the plate;
- laser therapy. Laser rays relieve pain, heal, stop inflammation in the lumbar vertebrae;
- darsonvalization. This method is designed to improve blood circulation, dilate blood vessels, stimulate nerve endings;
- phonophoresis treats with ultrasound, stimulates blood flow to the muscles in the dorsal.
Each method has its own contraindications. More difficult with traditional medicine. The official medicine still does not realize that the midwife knows how to treat lumbar osteochondrosis. Therefore, if a friend advises you to use a compress made with burdock broth, a pine bath, you should see a doctor. For anesthesia, methods such as hirudotherapy are used, but leeches hide behind this name, so doctors advise to use this method of treatment with caution.
Surgical troubleshooting
In some cases, it can no longer be done without surgery. With advanced intervertebral hernias, neurosurgeons use microdisceectomy. The operation removes the damaged disk. If there are no contraindications, then the doctor can perform nucleoplasty, which has many advantages:
- Does not require cutting;
- The operation takes up to 30 minutes;
- There are no restrictions on surgical procedures.
Important. To maintain the movement of the spine, strengthen the back muscles, it is recommended to do yoga, swimming, Pilates. Running produces a shock load on the vertebrae, so at the first sign of lower back pain, jogging should be abandoned.













































